Definition: Recurrence of clinical symptoms due to reactivation of pre-existent HSV-1 or HSV-2 infection after a period of latency.
| KEY POINTS |
|---|
| Most herpes recurrences are mild and infrequent and supportive care is all that is needed. |
| 43% of patients with genital HSV-1 will not get another recurrence after the first year of their initial outbreak.(1) |
| Management options are; supportive cares, episodic or suppressive medication. A patient-clinician partnership is the best way to arrive at an individualised treatment plan. |
| Suppressive treatment is useful for lessening recurrences and transmission as well as reducing patient distress and should be considered for anyone with recurrent genital herpes. |
| Some people may have a breakthrough recurrence while being on suppression therapy, if this occurs the antiviral dose can be increased. |
| Withdrawal of suppressive therapy should take place for a period that is sufficient to establish whether the pattern of recurrence has changed or at least 2 recurrences. |
History, examination and diagnosis
History
In straightforward cases, with a prior laboratory-confirmed diagnosis of HSV, clinical history is often the main way of determining the presence of a recurrent episode. Only 10–25% of individuals who are HSV-2 seropositive report a diagnosis of genital herpes, which suggests that most have unrecognised symptomatic or completely asymptomatic infections.(2) However, after being told that they are HSV-2 seropositive, more than 60% of individuals are able to identify clinically symptomatic recurrences that they may have previously been thought to be due to other conditions. See Figure 2 for a visual aid of these statistics.
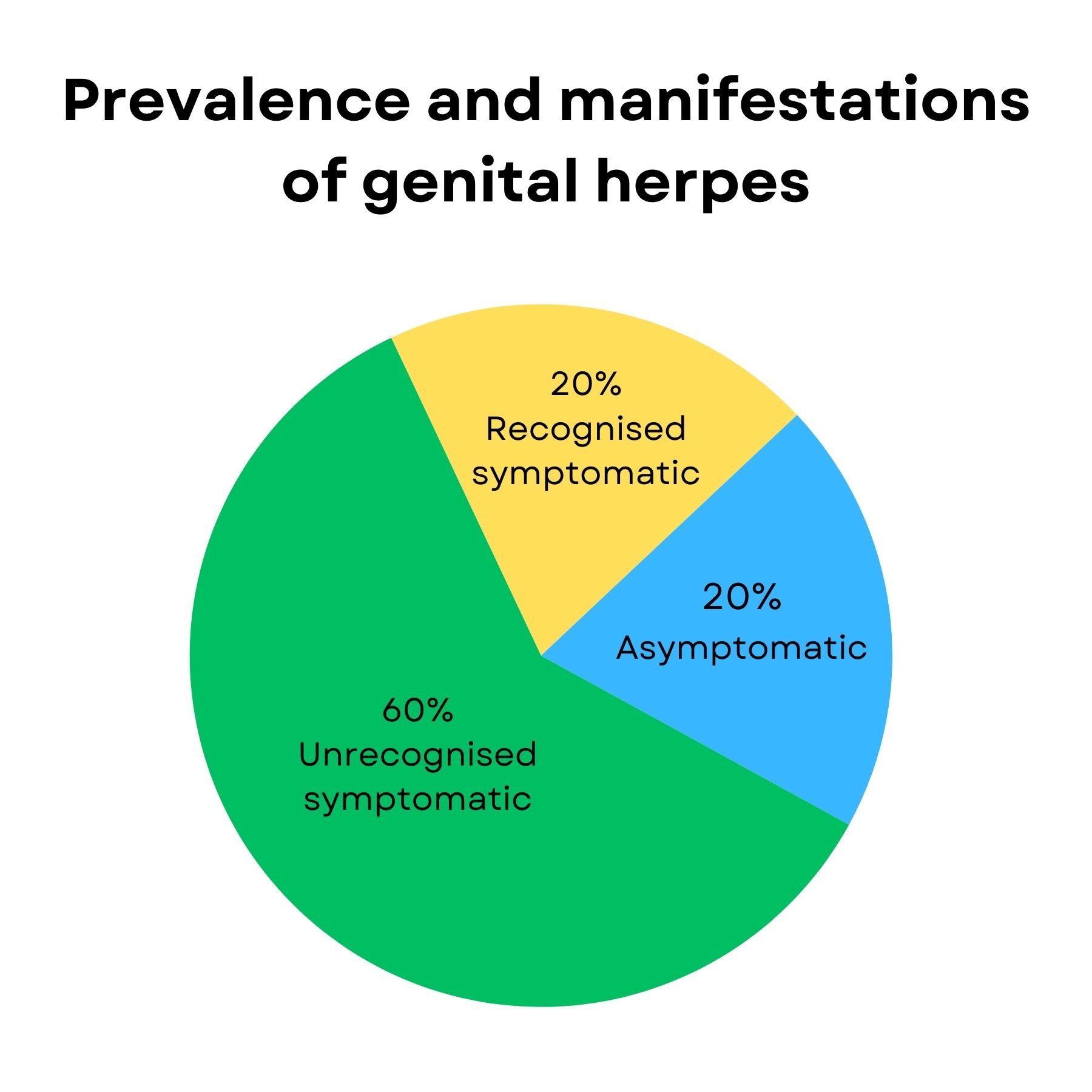
Figure 2. The percentage of people who are serologically positive for genital herpes HSV-2 and their clinical manifestations.(2)
Physical examination
Atypical presentation is not unusual and HSV should be considered in any recurrent intermittent inflammatory genital lesions, regardless of appearances. Any recurring lesion in the genital area that is 1-2 mm in size is strongly suggestive of HSV infection. Other genital conditions may mimic and/or coexist with recurrent herpes. GRADE C
Diagnosis
All genital lesions not previously diagnosed should have a HSV PCR swab taken. GRADE B However, it is important to note that the viral load is typically lower in recurrences of genital herpes compared with the first episode. Laboratory tests for HSV also have a significant false-negative rate, although this is less of an issue for genital swab PCR. The best method of obtaining virologic confirmation during a recurrence is to take a swab within 24 hours of symptom development and analyse using PCR. GRADE B In suspected recurrent infection a patient-taken swab at home is often more successful at showing HSV than a later clinician obtained PCR swab. Other causes of recurrent genital lesions should be considered, but if PCR remains negative despite the presence of continuing recurrent lesions then type-specific herpes serology testing may aid diagnosis and referral to a Sexual Health specialist.
Differential diagnoses
The following common conditions can be mistaken for genital herpes recurrences; lichen sclerosus, fissuring due to candidiasis, folliculitis, bacterial skin infections and dermatitis.
Less common differential diagnosis include; erythema multiforme, hidradenitis suppurativa, Epstein-Barr virus, fixed drug eruption, herpes zoster, aphthous ulcers and rarely autoimmune blistering disease.
Complications of recurrent genital herpes
- Lumbosacral radiculopathy can recur (but usually with less severe symptoms compared to the primary HSV infection). Gabapentinoids or tricyclic antidepressants have been found to be effective and generally well tolerated.
- Recurrent, benign, aseptic meningitis (Mollaret’s meningitis) may occur in individuals infected with HSV-2. Those affected should be offered long-term suppressive antiviral management, which may need to be continued indefinitely.
- Erythema multiforme, which can develop 3–14 days after HSV infection. Characterised by target lesions which typically resolve within 7-10 days. Recurrent episodes can be managed with continuous antiviral suppression treatment, consult with a specialist if indicated.
- Recurrent proctitis, suggested management includes supportive cares and continuous antiviral suppression treatment, consider consulting with a specialist if indicated.
A referral to a specialist is recommended for a patient with complications of HSV.
Treatment of recurrent genital herpes
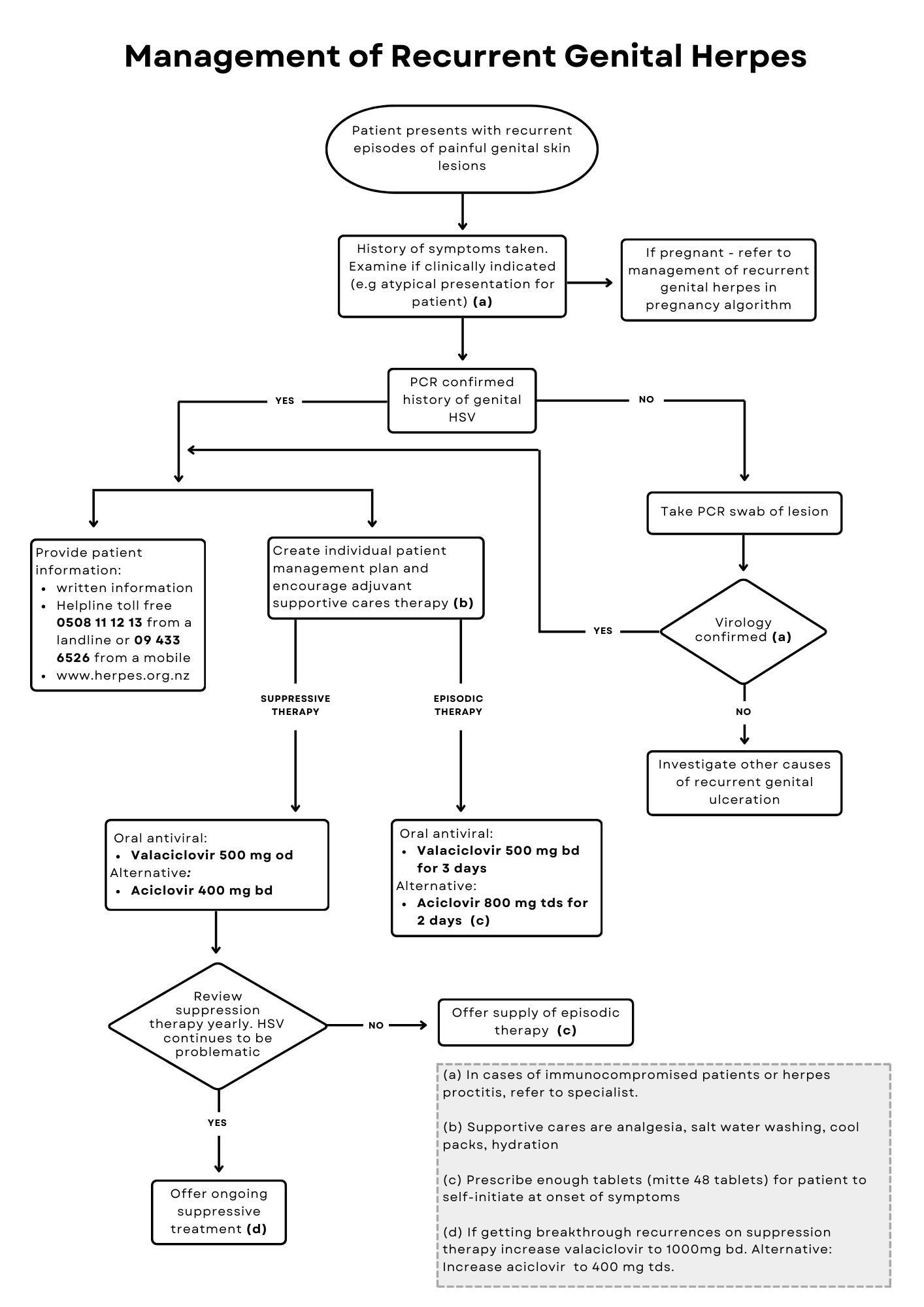
A treatment algorithm for recurrent genital herpes is shown in Figure 3.
The best strategy for managing an individual patient may change over time according to their recurrence frequency, symptom severity, and relationship status. Patient preference for how they wish to manage their herpes should be considered.
Strategies include:
- Supportive cares only.
- Episodic antiviral therapy.
- Suppressive antiviral therapy (short courses or continuous).
These strategies can be used in isolation or in conjunction with each other to individually tailor a management plan to a patient’s circumstances.
Supportive cares
Many patients choose to not use antiviral medication as their recurrences are rare and mild. Supportive cares include pain relief, micturition cares and salt water washes. (Refer to patient handout with supportive cares) Many people with HSV1 associated genital herpes will have no further recurrences after the first initial episode.
Episodic antiviral therapy
The aim of episodic treatment is to reduce symptoms and the duration of viral shedding during recurrences rather than to reduce the frequency of recurrences. The use of oral aciclovir or valaciclovir reduces the duration of an outbreak by a median of 1-2 days. A third of patients who use episodic antiviral medications reported that they were able to abort lesions appearing if they started treatment during the prodrome that precedes some outbreaks or within one day of lesion onset.(3, 4)
Episodic treatment may be preferable to continuous suppression therapy in individuals who have a well-recognised prodrome and/or less frequent recurrences and are in a relationship where the virus is shared.
Episodic antiviral medication
Preferred regimen:
- Valaciclovir 500 mg twice daily for 3 days
Alternative regimen:
- Aciclovir 800 mg three times daily for 2 days
Immunocompromised individuals (under specialist guidance):
- Valaciclovir 500 mg twice daily for 5 days
OR:
- Aciclovir 400 mg three times daily for 7-10 days
For episodic therapy to be effective sufficient quantities of medication need to be prescribed with instructions to start treatment as soon as symptoms begin. GRADE A
Suppressive antiviral therapy
Suppressive therapy refers to continuous oral antiviral therapy taken over a specific period of time; this effectively reduces the frequency of recurrences and lowers the risk of transmission.(5, 6) GRADE A Virological confirmation of the diagnosis is advised before starting suppressive antiviral therapy. Individuals with indicative symptoms, but no virological conformation should be referred to a sexual health specialist. The main aims of suppressive therapy is to improve the quality of life of people with recurrent genital herpes,(7, 8) as it lessens recurrences and reduces the risk of transmission. Suppression can either be taken for short courses or continuously. Short courses are specific time frames to support patients, for example, over high stress periods or while away on holiday. Clinicians need to note that full suppressive effect is usually only obtained five days into treatment.
Aciclovir and valaciclovir both suppress symptomatic and asymptomatic viral shedding by 80–95%.(9) Suppressive therapy with once-daily valaciclovir has been shown to reduce transmission to an uninfected partner, with a 48% reduction in acquisition of HSV infection and a 75% reduction in the rate of clinically symptomatic genital herpes.(10) Patients may consider suppressive antiviral therapy as a useful adjunct to safer sex behaviour, including the use of condoms, for the prevention of genital herpes transmission. Specialist supervision is indicated for management of suppression therapy in immunocompromised people.
Suppressive antiviral medication regimen
Preferred regimens:
- Valaciclovir 500 mg once a day
If recurrences not well controlled on this regime then consider changing to:
- Valaciclovir 500 mg twice daily
Alternative regimens:
- Aciclovir 400 mg twice daily
If recurrences not well controlled on this regime then consider changing to:
- Aciclovir 400 mg three times daily
Immunocompromised individuals (under specialist guidance):
- Valaciclovir 500 mg twice daily
Alternative regimens:
- Aciclovir 400 mg twice - three times daily
Prescribing should be reviewed after 12 months to see if patients' circumstances have changed and to explore if patients would like to come off suppressive therapy. Withdrawal of suppressive therapy should take place for a period that is sufficient to establish whether the pattern of recurrence has changed or at least 2 recurrences.
GRADE C
Some patients may choose a shorter suppressive course depending on their social circumstances. Suppressive therapy does not alter the long-term natural history of recurrences and it is common to have a recurrence soon after therapy withdrawal. Consider the provision of episodic therapy so patients can use episodic treatment during the suppression free trial period.
Some patients may need to be on suppressive therapy for years. Valaciclovir is well tolerated, and safety and efficacy data are supportive of longer-term use.(11) The dosage of valaciclovir or aciclovir should be reduced in the presence of severe renal failure. It is strongly advised to have virological confirmation of the diagnosis before starting suppressive antiviral therapy. Individuals with indicative symptoms of genital herpes who do not have virological confirmation of recurrences, or those with herpes-related complications or ongoing issues should be referred to a Sexual Health specialist.
Alternative genital herpes therapies
Topical aciclovir, in over the counter cold sore treatments, is less effective than oral aciclovir,(12) and therefore use of topical treatment is not recommended. Many alternative treatments (e.g. oral L-lysine, aspirin, liquorice root cream, lemon balm, aloe vera cream, etc.) to lower recurrences have been advocated but clinical trial data is not sufficient to recommend any of them.
Genital herpes in immunocompromised individuals
Although rare in immunocompetent individuals, clinically refractory (large, severe and sometimes atypical) genital herpes lesions may occur in patients with severe immunodeficiency, including late stage HIV disease. Immunocompromised individuals should be referred for specialist care.
References
- Engelberg R, Carrell D, Krantz E, et al. Natural history of genital herpes simplex virus type 1 infection. Sex Transm Dis 2003; 30 (2): 174-7.
- Wald A, Zeh J, Selke S, et al. Reactivation of genital herpes simplex virus type 2 infection in asymptomatic seropositive persons. N Engl J Med 2000; 342 (12): 844-50.
- Aoki FY, Tyring S, Diaz-Mitoma F, Gross G, et al. Single-day, patient-initiated famciclovir therapy for recurrent genital herpes: a randomized, double-blind, placebo-controlled trial. Clin Infect Dis 2006; 42 (1): 8-13.
- Tyring SK, Douglas JM, Jr., Corey L, et al. A randomized, placebo-controlled comparison of oral valacyclovir and acyclovir in immunocompetent patients with recurrent genital herpes infections. The Valaciclovir International Study Group. Arch Dermatol 1998; 134 (2): 185-91.
- Kaplowitz LG, Baker D, Gelb L, et al. Prolonged continuous acyclovir treatment of normal adults with frequently recurring genital herpes simplex virus infection. The Acyclovir Study Group. JAMA 1991; 265 (6): 747-51.
- Mertz GJ, Eron L, Kaufman R, et al. Prolonged continuous versus intermittent oral acyclovir treatment in normal adults with frequently recurring genital herpes simplex virus infection. Am J Med 1988; 85 (2A): 14-9.
- Patel R, Tyring S, Strand A, et al. Impact of suppressive antiviral therapy on the health related quality of life of patients with recurrent genital herpes infection. Sex Transm Infect 1999; 75 (6): 398-402.
- Romanowski B, Marina RB, Roberts JN. Patients' preference of valacyclovir once-daily suppressive therapy versus twice-daily episodic therapy for recurrent genital herpes: a randomized study. Sex Transm Dis 2003; 30 (3): 226-31.
- Wald A, Corey L, Cone R, et al. Frequent genital herpes simplex virus 2 shedding in immunocompetent women. Effect of acyclovir treatment. J Clin Invest 1997; 99 (5): 1092-7.
- Corey L, Wald A, Patel R, et al. Once-daily valacyclovir to reduce the risk of transmission of genital herpes. N Engl J Med 2004; 350 (1): 11-20.
- Tyring SK, Baker D, Snowden W. Valacyclovir for herpes simplex virus infection: long-term safety and sustained efficacy after 20 years' experience with acyclovir. J Infect Dis 2002; 186 (Suppl 1): S40-6.
- Trottet L, Owen H, Holme P, et al. Are all aciclovir cream formulations bioequivalent? Int J Pharm 2005; 304 (102): 63-71.